Replacing defective neurons is an attractive goal in diseases such as Parkinson's disease or ALS, but one that still seemed unrealistic. Recently impressive progress has been made.
Parkinson's disease is a neurodegenerative disorder caused by the selective degeneration of dopaminergic cells in the substantia nigra leading to major problems in the motor system. The substancia nigra is a tiny part of the mid brain.
 Source Wikipedia: FrozenMan - Own work
Source Wikipedia: FrozenMan - Own work
One futuristic therapeutic approach for Parkinson's disease is dopaminergic cell-replacement therapy, in which dopaminergic precursors are grafted into the striatum to restore the lost dopaminergic neurotransmission.
Previous clinical trials based on foetal dopamine neuron transplantation have shown promising results, but also significant limitations including the survival of grafted dopaminergic neurons, which is very poor.
A major limiting factor for cell therapy in Parkinson's disease is the poor survival and reinnervation capacity of grafted dopaminergic neurons.
Major factors responsible for the high levels of dopaminergic cell loss during the transplantation process and early post-transplantation period have not been totally clarified. However, grafting-related cell trauma, lack of growth factors, poor vascularization, neuroinflammation and other factors have been involved.
MSCs have been effective against several of the above-mentioned factors, and a neuroprotective effect on grafted dopaminergic neurons could be expected. Mesenchymal stromal cells are multipotent cells originally isolated from the stroma of the bone marrow. Different studies have shown their capability to regulate the local environment through the release of immunomodulatory, antiapoptotic and trophic factors. These properties make them an attractive cell source for repairing damaged tissue.
In this work, Jannette Rodriguez-Pallares and colleagues from Spain, investigated whether co-grafting of MSCs could improve the survival and reinnervation ability of dopaminergic precursors transplanted in animal models of Parkinson's disease.
Rats with total unilateral dopaminergic denervation were grafted with a cell suspension of rat dopaminergic precursors (500,000 cells) with or without a high (200,000 cells) or low (25,000 cells) number of MSCs. Eight weeks after grafting, rats were tested for motor behaviour and sacrificed for histological analysis.
Results showed that the survival of dopaminergic neurons and graft-derived striatal dopaminergic innervation was higher in rats that received co-grafts containing a low number of MSCs than in non-co-grafted controls.
Surprisingly, the increase in the number of co-grafted MSCs led to detrimental effects. The mechanisms responsible for this effect are still unclear. A high concentration of MSCs may induce MSC senescence, damaged mitochondrial transfer or dysregulation of pro-inflammatory cytokine production.
In conclusion, co-grafting with MSCs or MSCs-derived products may constitute a useful strategy to improve dopaminergic graft survival and function. However, a tight control of MSCs density or levels of MSCs-derived products is necessary.
Read the original article on Pubmed

 Source: KieranMaher at English Wikibooks
Source: KieranMaher at English Wikibooks
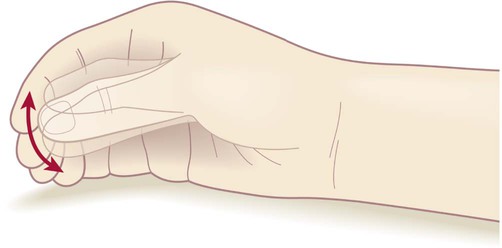 ‘Pill-rolling’ rest tremor as found in Parkinson’s disease.
‘Pill-rolling’ rest tremor as found in Parkinson’s disease. Source Wikipedia: FrozenMan - Own work
Source Wikipedia: FrozenMan - Own work