I am somewhat skeptical about the benefits of acupuncture beyond the placebo effect. However, this article suggests it could be beneficial for individuals with Parkinson's disease.
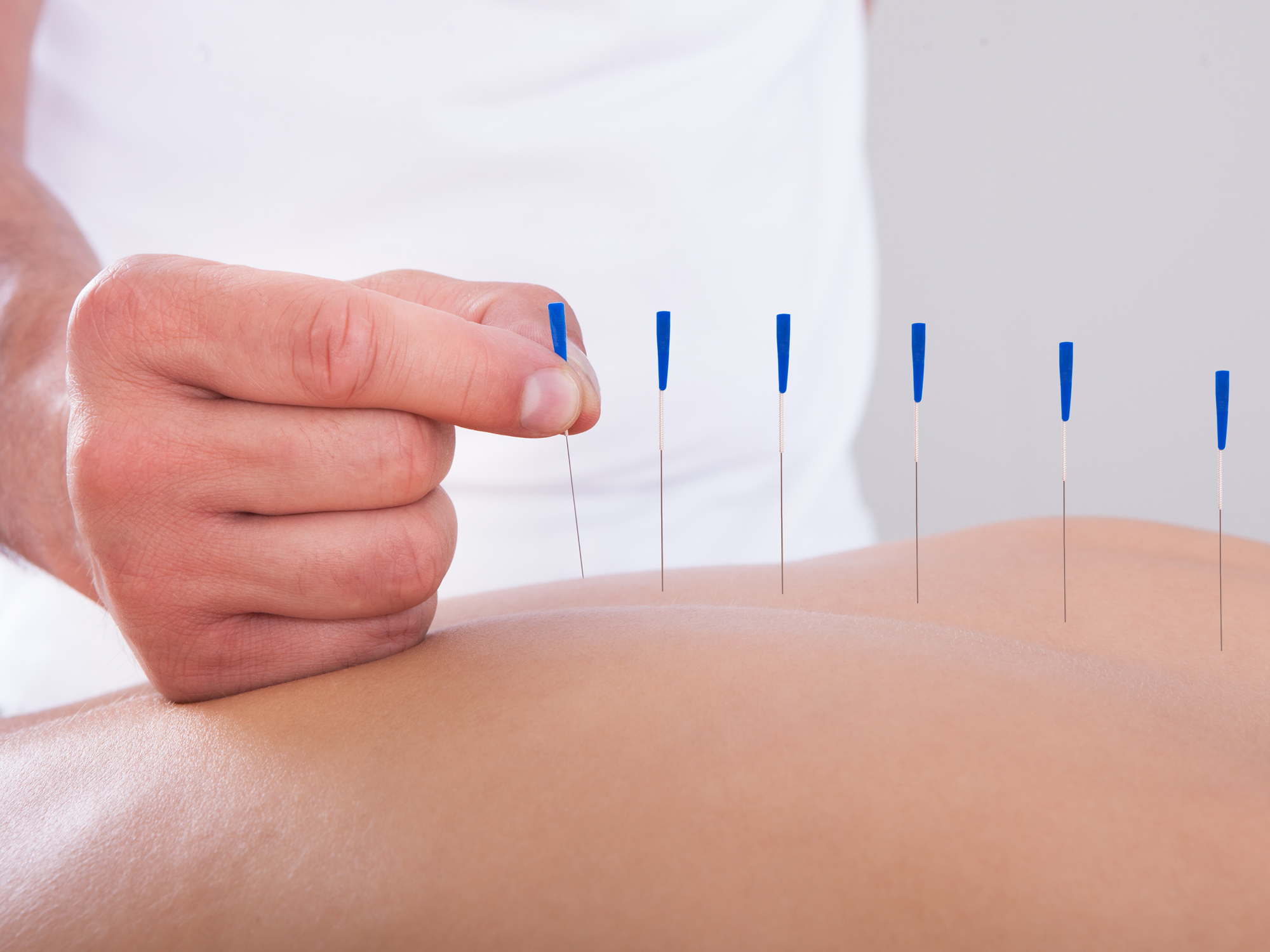 This study investigates whether acupuncture has any impact on long-term health outcomes, such as mortality, disease progression, or complications, in individuals newly diagnosed with Parkinson’s disease (PD) in South Korea. Indeed, it is unclear what constitutes an effective acupuncture session for Parkinson's disease, and individuals interested should receive at least one session every two months. It is commonly believed that in PD, reduced mobility due to tremors, postural imbalance, and rigidity likely contributes to poor circulation and decreased gastrointestinal motility, leading to bowel obstructions and impaired swallowing, which can, in turn, result in recurrent aspiration pneumonia. The benefits may arise from the fact that people with PD might find it easier to move.
This study investigates whether acupuncture has any impact on long-term health outcomes, such as mortality, disease progression, or complications, in individuals newly diagnosed with Parkinson’s disease (PD) in South Korea. Indeed, it is unclear what constitutes an effective acupuncture session for Parkinson's disease, and individuals interested should receive at least one session every two months. It is commonly believed that in PD, reduced mobility due to tremors, postural imbalance, and rigidity likely contributes to poor circulation and decreased gastrointestinal motility, leading to bowel obstructions and impaired swallowing, which can, in turn, result in recurrent aspiration pneumonia. The benefits may arise from the fact that people with PD might find it easier to move.
As is often the case, the Korean authors used a database to select patients and gather information about their health over the following years. They did not see any patients in person; it was purely a matter of processing numbers in the database. The NHIS database contains extensive patient information, including diagnostic codes, healthcare utilization, prescriptions, vital signs, disability grades, sex, age, and socioeconomic factors such as health insurance. However, this database does not provide precise medical details.
Who Was Included in the Study?
The study focused on adults (age 19 or older) newly diagnosed with idiopathic Parkinson’s disease (IPD) between 2012 and 2016.
To ensure a cleaner analysis, the authors excluded individuals diagnosed with Parkinson’s before 2012 or who were disabled at the time of diagnosis. They also excluded patients diagnosed with dementia or who died within a year of their diagnosis. To strengthen the results, they excluded patients who had received acupuncture in the six months preceding their diagnosis.
After applying these exclusions, about 41,000 patients remained. From this group, the researchers employed "propensity score matching" to pair patients from both groups who had similar health and demographic profiles (like age, sex, income, location, and other health conditions). After further exclusions and matching, 6,394 patients remained in each group.
The researchers measured all-cause mortality (death from any cause), tracked for up to six years following diagnosis. They also recorded fractures (such as hip or spine fractures), emergency room visits, and deep brain stimulation (DBS) surgery. These outcomes serve as proxies to assess whether acupuncture is associated with slower disease progression or fewer complications.
How Were Acupuncture and Non-Acupuncture Groups Defined?
Acupuncture was counted only if a person had six or more sessions in the year following diagnosis. This cutoff is based on previous studies suggesting that at least six sessions may be necessary to observe an effect. The acupuncture types included conventional methods as well as specialized forms like ocular or electroacupuncture.
Results:
Overall, the mortality in the acupuncture group (960) was significantly lower than in the control group (1,118). Deaths due to neoplasms (174 vs 234), circulatory (172 vs 208), and digestive diseases were also lower in the acupuncture group. In all cases, the acupuncture group had equal or better results than the control group. However, no significant differences were observed between groups in fracture risk, emergency room visits, or DBS procedures.
Key Takeaways
The study aimed to explore whether acupuncture might influence survival or disease progression in Parkinson’s disease. To achieve this, it utilized a large, high-quality national health dataset and careful matching to compare similar patients. While the text does not cover the results themselves (e.g., whether acupuncture improved survival or reduced complications), the methods ensure that any differences found are likely due to the treatment rather than other health or demographic factors.
