Nervous system injuries affect over 10 of thousands people every year. It is estimated that spinal cord injuries alone affect 10,000 each year. Nervous system injuries includes also effects of stroke, glaucoma and some injuries to the eye.
The nervous system is divided into two parts: the central nervous system, which consists of the brain and spinal cord, and the peripheral nervous system, which consists of cranial and spinal nerves along with their associated ganglia.
Nerve regeneration (the regrowth or repair of nervous tissues), a subfield of neural tissue engineering, is becoming a rapidly growing field dedicated to the discovery of new ways to recover nerve functionality after injury. However neuroregeneration differs between the peripheral nervous system (PNS) and the central nervous system (CNS). When an axon is damaged, the distal segment undergoes Wallerian degeneration, while the proximal segment can either die by apoptosis or undergo the chromatolytic reaction, which is an attempt at repair.
There is currently no treatment for recovering human nerve function after injury to the central nervous system. Unlike peripheral nervous system injury, injury to the central nervous system is limited by the inhibitory growth environment which is, in part, created by the migration of myelin-associated inhibitors, astrocytes, oligodendrocytes, oligodendrocyte precursors, and microglia.
Although neuroinflammation is often depicted as detrimental, there is growing evidence that alternatively activated, reparative leukocyte subsets and their products can be deployed to improve neurological outcomes.
Using a mouse model, researchers at Ohio State and the University of Michigan discovered a new type of immune cell that not only rescues damaged nerve cells from death, but partially reverses nerve fiber damage. The research team also identified a human immune cell line, with similar characteristics, that promotes nervous system repair.
The cell discovered by these researchers is a granulocyte, a type of white blood cell that has small granules. The most common granulocytes, neutrophils, normally help the body fight off infection. The unique cell type resembles an immature neutrophil but is distinctive in possessing neuroprotective and neuroregenerative properties. It drives central nervous system axon (nerve) regrowth in vivo, in part through the secretion of a cocktail of growth factors.
In the current study, the researchers identify a unique granulocyte subset, with characteristics of an immature neutrophil, that had neuroprotective properties and drove CNS axon regeneration in vivo, in part via secretion of a cocktail of growth factors. This pro-regenerative neutrophil promoted repair in the optic nerve and spinal cord, demonstrating its relevance across CNS compartments and neuronal populations. Their findings could lead to the development of new therapies that reverse CNS damage and restore lost neurological function across a spectrum of diseases.
The researchers demonstrated the therapeutic potency of the immature neutrophils subset by injecting them into mice with crush injury to the optic nerve or lacerated nerve fibers in the spinal cord. Mice injected with the new neutrophil subset, but not more typical mature neutrophils, grew new nerve fibers.
The next step for the Ohio State and University of Michigan researchers is to collect the neuro-enhancing granulocytes they discovered and figure out how to enhance them in the lab. Ultimately, they hope to determine whether the cells could be injected into patients to reverse damage to the central nervous system.
"Our findings could ultimately lead to the development of novel immunotherapies that reverse central nervous damage and restore lost neurological function across a spectrum of diseases," said first author Dr. Andrew Sas, an assistant professor and physician scientist in the Department of Neurology at Ohio State.
Dr. Benjamin Segal, professor and chair of the Department of Neurology at The Ohio State College of Medicine and co-director of the Ohio State Wexner Medical Center's Neurological Institute said: "In the future, this line of research might ultimately lead to the development of novel cell based therapies that restore lost neurological functions across a range of conditions."


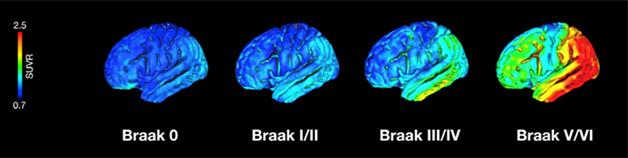 Source Alzforum
Source Alzforum
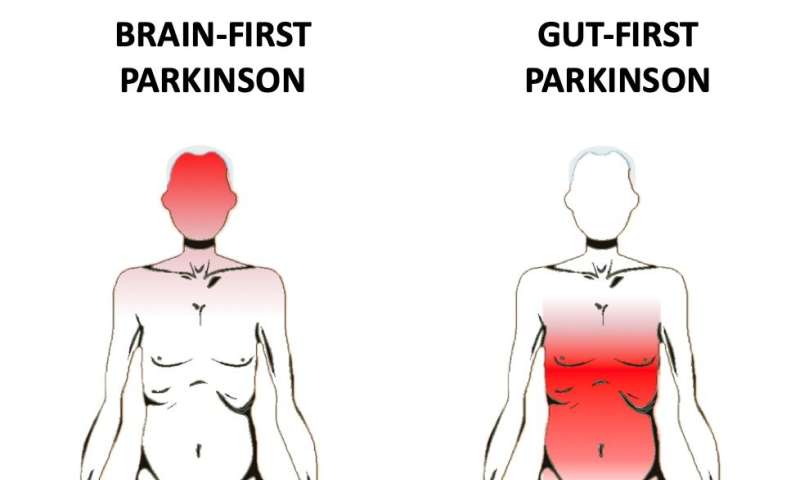
 The substantia nigra in the brain.
Source Wikipedia
The substantia nigra in the brain.
Source Wikipedia The pons area in the brain.
Source Wikipedia
The pons area in the brain.
Source Wikipedia