The theory of infectious origin of the Alzheimer's disease
The hypothesis that Alzheimer's disease has an infectious origin, has a long and controversial history. The data at the origin of this hypothesis are contradictory and mainly associative in nature, without it being possible to demonstrate a causal link. Interest in this theory has been renewed, however, by several recently published observations. In the section Viewpoint de la revue Nature Reviews Neurology, Ben Readhead, a researcher at the Biodesign Institute's ASU-Banner Center for Research on Neurodegenerative Diseases, joined several distinguished colleagues to discuss the idea that bacteria, viruses or other infectious pathogens can play a role in Alzheimer's disease.
First, it has been shown that the amyloid β can act as an antimicrobial peptide and that selected microorganisms can seed the deposition of Aβ in mouse models.
Second, genetic data has rekindled interest in the role of herpesviruses, in particular the human Herpes 6 virus (HHV6), in Alzheimer's disease.
Third, the epidemiological data from Taiwan suggests that antiherpetic drugs reduce the risk of dementia.
Preclinical data have indicated that microorganisms associated with periodontal disease may contribute to the pathology of Alzheimer's disease.
Finally, genetic, pathological and modeling studies of Alzheimer's disease have shown that the immune system plays an important role in Alzheimer's disease.
A hypothesis that has never been favored by researchers
This hypothesis may have been rejected too quickly. For example, microorganisms do not only cause acute illnesses, in fact certain microorganisms can hide in the body for decades in latent form, causing damage intermittently or after long periods of silence.
In addition, being infected does not necessarily mean being symptomatic. For example, out of the millions of people infected with Mycobacterium tuberculosis, only about a tenth of them will develop tuberculosis. Likewise, most people infected with HSV1 do not develop cold sores so it is possible that asymptomatic carriers of this virus were often mistakenly included in the control groups. It should also be noted that many viruses of the Herpes family (HSV1, HSV2, VZV) live preferentially in neurons.
A role for an infectious agent - in particular the herpes simplex 1 virus (HSV1) - in Alzheimer's disease (Alzheimer's disease) was proposed about 30 years ago based discovery of HSV1 DNA in the brain tissue of a large proportion of the elderly, followed by evidence that e the virus confers a high risk of disease to carriers of the ε4 allele of the gene apolipoprotein E (APOE * ε4).
Shortly after the detection of HSV1 DNA, two different species of bacteria, Borrelia burgdorferi and Chlamydia pneumoniae, were implicated in Alzheimer's disease, and a third species, Porphyromonas gingivalis, was recently added to the list.
Doubts remain, however
Nevertheless, it is known that an acute end-of-life infection, such as pneumonia, can cause a dramatic increase in the amount of microorganisms in the brain. They will then be detected post-mortem but that does not mean that these microorganisms are at the origin of the Alzheimer's disease. In addition, the issue of reverse causation is never really addressed: For example, clinical Alzheimer's disease can lead to poor dental hygiene and, therefore, damage to the oral microbiome.
Indeed, there are many challenges to prove the theory of microbial origin of Alzheimer's disease. A potential challenge is that each drug has a relatively narrow spectrum of antimicrobial activity. However, since a large number of microorganisms have been associated with Alzheimer's disease by a range of researchers, it would be difficult to interpret what a negative result in a clinical trial would mean, which would necessarily use a specific antimicrobial.
Another problem is the duration of the disease. We know that the underlying pathology of Alzheimer's disease begins 20 years or more before the onset of symptoms. So, how to prove that an infectious process that occurred decades before the onset of symptoms, really contributed to the disease process?
One may also wonder why bacteria or viruses would escape the innate innate immune defense mechanisms, which are responsible for protecting the brain against such an invasion.








 Source: Вых Пыхманн via Wikipedia
Source: Вых Пыхманн via Wikipedia Classical conception of the metastasis process
Source: doi: 10.1038 / nri3789
Classical conception of the metastasis process
Source: doi: 10.1038 / nri3789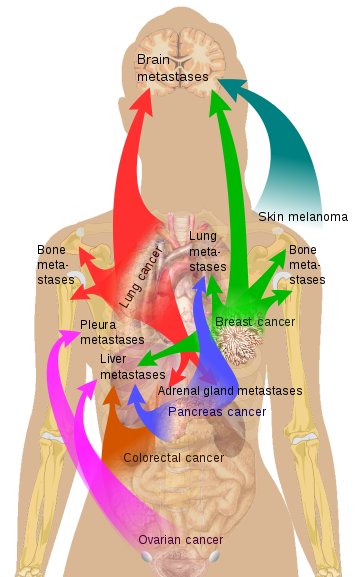 Source Mikael Häggström via Wikipedia
Source Mikael Häggström via Wikipedia