Nearly 3 out of 4 cancer patients undergoing chemotherapy suffer from loss of memory, attention or concentration. This range of cognitive deficiencies referred to as chemotherapy-induced cognitive impairment, chemobrain or chemofog severely hampers quality of life of patients undergoing treatment. Advanced neuroimaging analyses have identified structural white and gray matter damage following chemotherapy in patients treated for various types of cancer. Cognitive deficits associated with platinum-based therapeutics such as cisplatin have been observed for 5-10 years post-diagnosis. However, no United States Food and Drug Administration-approved therapeutic interventions are available to date.
Mitochondrial dysfunction, characterized by abnormal morphology, impaired bioenergetics, altered mitochondrial dynamics and mitochondrial DNA mutations, has emerged as an underlying mechanism of several pathologies, including neurodegenerative diseases, cerebral and cardiac ischemia , traumatic brain injury, spinal cord injury, cancer, and chemotherapy-induced cognitive impairment and peripheral neuropathy. Following cerebral ischemia, astrocytes donate their healthy mitochondria to ischemic neurons with dysfunctional mitochondria to maintain adequate mitochondrial function and survival.
Studies in the 1930s already showed that nasally administered bacteria can cross the nasal epithelium within minutes, indicating a paracellular route of entry.
In a recent study, Jenolyn F. Alexander, Cobi J. Heijnen and colleagues demonstrated that nasal administration of mesenchymal stem cells restores cisplatin-induced cognitive impairment in mice and their data indicated that these mesenchymal stem cells act by repairing neuronal mitochondrial damage.

It appeared that autologous mesenchymal stem cells work as well as human mesenchymal stem cells in their mouse model. The concept of mitochondrial administration is also being considered the treatment of Parkinson's disease, cerebral and cardiac ischemia, cancer, diabetic nephropathy and spinal cord injuries and some clinical trials for evaluating the safety and efficacy of isolated mitochondria based therapies have also recently commenced.
These findings indicate that cisplatin-induced accumulation of mitochondrial p53 is the cause of the damage to brain mitochondria that leads to cognitive deficits in response to treatment with this chemotherapeutic. The authors recently showed that astrocytes donate their healthy mitochondria and rescue primary cortical neurons damaged by cisplatin in vitro.
Based on their above-mentioned findings that mitochondrial deficits underlie cisplatin-induced neuronal damage and cognitive deficits, and that healthy mitochondria can be taken up by damaged neurons, the scientists hypothesized that isolated mitochondria from healthy mesenchymal stem cells can be used to resolve cisplatin-induced cognitive deficits and the associated structural damage. This would provide an advantage from the perspective of safety because the scientists do not need donation of allogeneic intact cells.
Mice were intraperitoneally injected with cisplatin at 2.3 mg/kg for 5 consecutive days, followed by 5 days of rest and another 5 days of cisplatin injection. The two administrations of mitochondria on mice delivered nasally, completely restored within two weeks mice's executive functioning, spatial recognition and working memory previously impaired by cisplatin treatment. The entry of mesenchymal stem cells into the brain is facilitated by pretreatment of the nasal cavity with hyaluronidase. The scientists maintained the mitochondria in calcium-free mitochondrial respiration buffer until ready for nasal delivery when they were transferred to calcium-free PBS.
Within 30 min of nasal administration, the mitochondria were detectable in the meninges where they were predominantly internalized by macrophages. Within this 30 min, the mitochondria also arrived at the ventricles and choroid plexus, gaining access to the brain.
3 h after delivery, mitochondria were found distributed along the rostral migratory stream where they were internalized by GFAP+ cells. By this time the nasally administered mitochondria also reached the hippocampus. Evidently, these mitochondria that had entered the meninges and brain completely restored the cisplatin-induced white matter damage in the cingulate cortex, synaptic loss in the hippocampus, and the compromised synaptosome membrane integrity and structural mitochondrial defects in synaptosomes as observed 35 days after the second mitochondrial donation.
The scientists used mitochondria isolated from human mesenchymal stem cells in their mouse model for the primary purpose of being able to trace the administered mitochondria with a human-specific mitochondrial antibody.
One topic of concern usually raised with the administration of isolated mitochondria is the possibility that they may function as damage-associated molecular proteins (DAMPs) which could lead to neuroinflammation. However, the scientists did not see activation of inflammatory pathways in the hippocampal transcriptome using human mitochondria. Mitochondria lack many surface antigens including HLA-Class 1 antigens thereby exhibiting lower immunogenicity than mesenchymal stem cells. This is one advantage favoring the clinical translation of allogeneic donation of mitochondria over mesenchymal stem cells.
An important benefit of their approach is the nasal route of delivery. In case of central nervous system (CNS)-targeted delivery of therapeutics, intracranial administration poses serious risk of injury. Intravenous administration has the disadvantage that it may lead to accumulation in the lung and liver requiring high doses which may generate inflammatory reactions or other adverse effects. Systemic administration of therapeutics intended to reach the brain are also obstructed by the blood-brain and blood-cerebrospinal fluid (CSF) barriers. In contrast, the nasal route of delivery is simple, non-invasive and facilitates the delivery of therapeutics to the brain thereby reducing the amount of mitochondria required.
Questions are raised on the ability of isolated mitochondria to survive in high extracellular calcium levels upon administration and to generate sufficient energy to enter cells and continue to function after cellular uptake. Upon internalization, mitochondrial donation enhanced the bioenergetics of the damaged cells for at least 21 days.
It is still unknown how donated mitochondria repair damaged neuronal cells. Interactions between mitochondrial and nuclear genes are vital for fundamental cellular processes such as respiration, transcription and translation. The authors observed that the internalized mitochondria, in many instances were localized close to the nucleus (perinuclear), as if communicating with them. In the literature it has been suggested that donated mitochondria can fuse with mitochondria of damaged recipient cells and thereby repair the bioenergetic machinery or replenish mitochondrial DNA in the acceptor cell.
Although this might be true, it remains difficult to accept that the few mesenchymal stem cells-derived mitochondria can restore cellular respiration by physical fusion to the many acceptor cell mitochondria. It is more likely that the donated mitochondria activate a transcriptional program leading to enhanced Nrf2 signaling and subsequent recovery of host mitochondrial function by a host of antioxidants.
Their findings elucidate the therapeutic effects of nasally delivered mitochondria to resolve unmet needs in the treatment of cancer survivors with neurotoxicities and highlights its potential significance for clinical translation. It also provides promise for treatment of a range of cognitive and neuronal deficits warranting further investigation in large animal models.



 Classical conception of the metastasis process
Source: doi: 10.1038 / nri3789
Classical conception of the metastasis process
Source: doi: 10.1038 / nri3789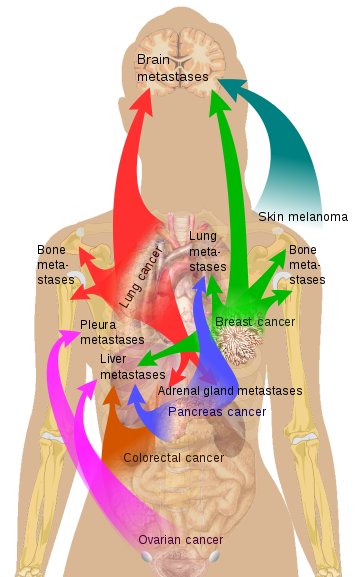 Source Mikael Häggström via Wikipedia
Source Mikael Häggström via Wikipedia * Zephyris Source CC BY-SA 3.0, * https://commons.wikimedia.org/w/index.php?curid=10811330
* Zephyris Source CC BY-SA 3.0, * https://commons.wikimedia.org/w/index.php?curid=10811330
