A Rare Gene Mutation Offers Clues to Combating Alzheimer’s and Cancer
The human immune system is not only our first line of defense against infectious threats, but it also plays an essential role in regulating how our bodies respond to internal dangers like cancer and neurodegenerative diseases.
One of the immune system’s tools is a molecular pathway known as cGAS-STING. This pathway functions as a sensor, detecting misplaced DNA in cells — a common feature in viral infections, cancer transformations, and some brain disorders.
A rare genetic mutation, first observed in 2019 in a woman with a strong inherited risk for Alzheimer’s disease, may help us better understand and even treat conditions such as Alzheimer’s, cancer, and autoimmune disorders. This woman, who carried a high-risk PSEN1 mutation that usually causes early-onset Alzheimer’s, remained cognitively intact into her seventies. Postmortem analysis revealed extensive amyloid plaques in her brain (a hallmark of Alzheimer’s) but very low tau pathology, which is more closely linked to memory loss and cognitive decline.
Genetic testing showed she carried two copies of a rare variant of the APOE3 gene: R136S, also known as the Christchurch mutation. APOE is a gene long known to influence Alzheimer’s risk, with different variants (APOE2, APOE3, and APOE4) conferring varying levels of protection or susceptibility.
What roles does the cGAS-STING pathway play? Under normal conditions, our cells keep their DNA tightly stored in the nucleus. But sometimes, DNA ends up in the wrong place — floating in the cytoplasm, the main body of the cell. This can happen due to viral infection, cellular stress, or genetic damage. The immune system interprets this misplaced DNA as a danger signal.
cGAS acts as a sensor activated primarily in two pathological contexts: microbial invasion by DNA viruses, bacteria, or retroviruses that introduce exogenous DNA into the cytoplasm, and aberrant leakage of nuclear or mitochondrial self-DNA into the cytosol. When cGAS detects double-stranded DNA in the cytoplasm, it produces a signaling molecule called cGAMP. This molecule then binds to a protein called STING (stimulator of interferon genes), activating a cascade that results in the production of type I interferons and inflammatory cytokines. These signals alert the immune system to potential threats and mobilize a defensive response. Interestingly, TDP-43, which is involved in several degenerative diseases, also has roles in protecting against DNA damage and viruses such as HIV.
While this response is critical for fighting infections and catching early-stage tumors, it can also become problematic when overactive. Persistent or misdirected cGAS-STING activity has been linked to autoimmune diseases, chronic inflammation, and cellular aging (senescence).
New Insights from Mouse Models To explore how exactly the R136S mutation offers protection, researchers engineered mice with human APOE3 or APOE3-R136S genes and introduced a tauopathy-causing mutation (P301S) mimicking key features of Alzheimer’s and frontotemporal dementia.
The findings were compelling: Mice carrying the R136S mutation showed less tau buildup, fewer signs of synaptic and myelin loss, and better brain activity patterns (theta and gamma oscillations important for learning and memory).
At the molecular level, the R136S mutation suppressed the cGAS-STING pathway in microglia, the brain’s resident immune cells.
When researchers treated APOE3 mice (a model of Alzheimer's) with a cGAS inhibitor, these animals exhibited many of the same benefits seen in people who are R136S carriers, including protection from tau-induced synaptic damage and similar gene expression changes across multiple brain cell types.
cGAS-STING: From Immunity to Neurodegeneration This research highlights a key insight: overactivation of cGAS-STING in microglia plays a damaging role in tau-driven neurodegeneration. Misfolded tau proteins can cause inflammation and disrupt brain networks, and microglia that respond too strongly—especially by ramping up interferon signaling through cGAS-STING—may inadvertently worsen the damage.
By reducing this response, the R136S mutation appears to create a more balanced immune environment in the brain. Instead of amplifying harmful inflammation, microglia can more effectively process and break down tau.

The discoveries related to R136S and the cGAS-STING pathway have broad implications:
- Cancer Immunotherapy: The same pathway that detects misplaced DNA in Alzheimer’s also helps identify cancer cells. Modulating cGAS-STING could improve immune responses against tumors or reduce chronic inflammation that promotes their growth.
- Autoimmune Disorders: Conditions like Aicardi–Goutières syndrome involve constant activation of the cGAS-STING pathway, leading the body to attack itself. Understanding how mutations like R136S impact this response may aid in developing treatments that dial down harmful immune activity without compromising protective responses.
- Healthy Aging and Senescence: The cGAS-STING pathway is also involved in cellular aging and the development of the senescence-associated secretory phenotype (SASP). Inhibiting this pathway could delay age-related degeneration and lessen age-related inflammation.
Looking Forward: From Mutation to Medicine
As discussed above, reducing cGAS-STING activity carries risks, including the potential to increase cancer susceptibility in older adults. Additionally, effects may vary across different cell types, benefiting the brain while impairing other vital organs. There are multiple schools of thought about what causes Alzheimer's disease; some incriminate the tau protein, but a majority of researchers are working on mitigating amyloid plaques. Another consideration —though obvious but not often explicitly stated— is that this research provides a preventive tool against Alzheimer's disease. In its early stages, it may slow the disease's progression, but it cannot cure someone who experiences the full impact of the disease.
In conclusion, the cGAS-STING pathway is a crucial sensor of misplaced DNA and a regulator of immune responses. A rare mutation in APOE3 (R136S) has been shown to suppress this pathway in brain immune cells, protecting against tau-related damage in Alzheimer’s models. This discovery opens new avenues for treating neurodegenerative diseases, autoimmune disorders, and cancer through precise modulation of our immune system’s ancient alarm system.

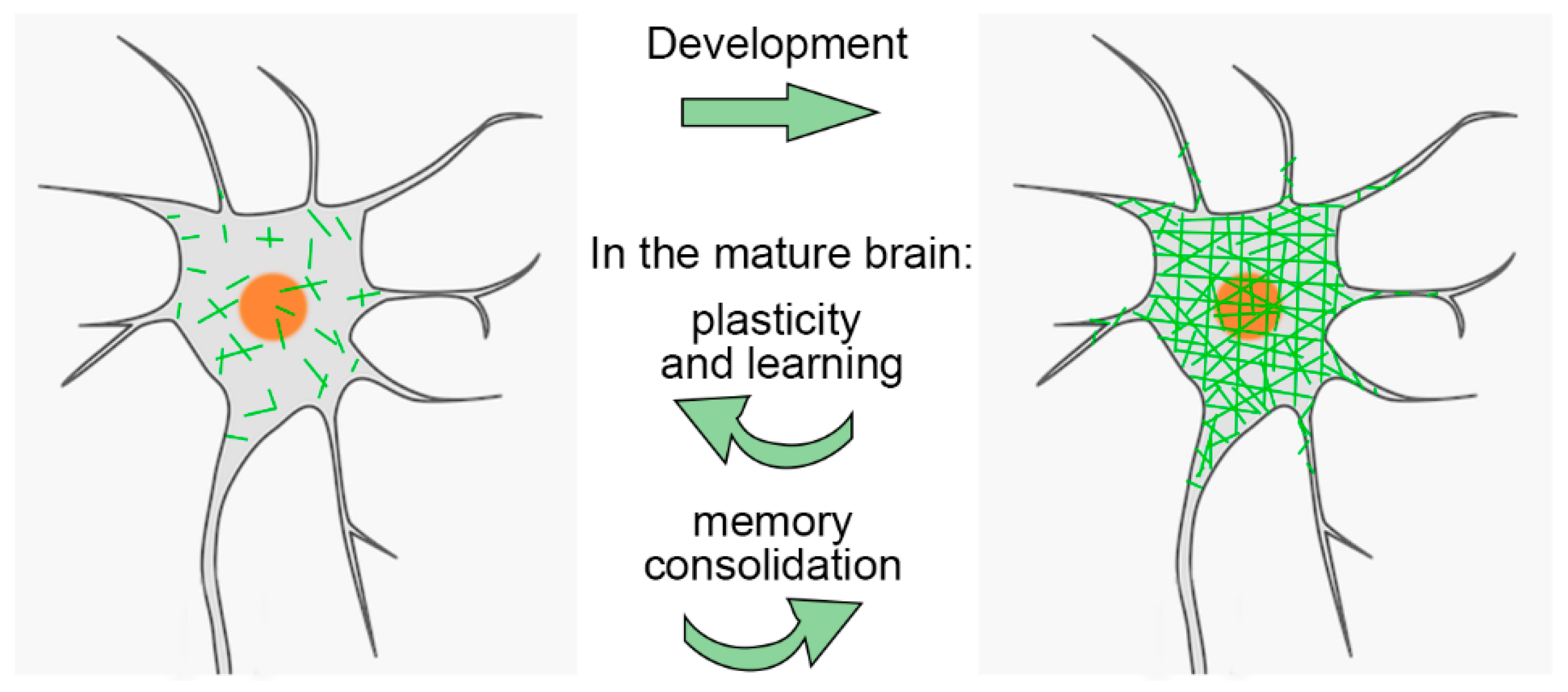 PNNs are especially important during brain development. They help close the "critical period" of heightened plasticity in childhood. Interestingly, while PNNs are degraded in adults, this plasticity can be partially restored. For example, PNN removal can promote recovery in stroke models
PNNs are especially important during brain development. They help close the "critical period" of heightened plasticity in childhood. Interestingly, while PNNs are degraded in adults, this plasticity can be partially restored. For example, PNN removal can promote recovery in stroke models This study investigates whether acupuncture has any impact on long-term health outcomes, such as mortality, disease progression, or complications, in individuals newly diagnosed with Parkinson’s disease (PD) in South Korea. Indeed, it is unclear what constitutes an effective acupuncture session for Parkinson's disease, and individuals interested should receive at least one session every two months. It is commonly believed that in PD, reduced mobility due to tremors, postural imbalance, and rigidity likely contributes to poor circulation and decreased gastrointestinal motility, leading to bowel obstructions and impaired swallowing, which can, in turn, result in recurrent aspiration pneumonia. The benefits may arise from the fact that people with PD might find it easier to move.
This study investigates whether acupuncture has any impact on long-term health outcomes, such as mortality, disease progression, or complications, in individuals newly diagnosed with Parkinson’s disease (PD) in South Korea. Indeed, it is unclear what constitutes an effective acupuncture session for Parkinson's disease, and individuals interested should receive at least one session every two months. It is commonly believed that in PD, reduced mobility due to tremors, postural imbalance, and rigidity likely contributes to poor circulation and decreased gastrointestinal motility, leading to bowel obstructions and impaired swallowing, which can, in turn, result in recurrent aspiration pneumonia. The benefits may arise from the fact that people with PD might find it easier to move. By Manu5 - http://www.scientificanimations.com/wiki-images/
By Manu5 - http://www.scientificanimations.com/wiki-images/