The reason we need sleep seems clear: without sleep, we become tired, and irritable and our brain functions less well. Conversely, after a good night's sleep, the brain and body feel refreshed. But why does the brain need to disconnect from the environment for hours every day? What is restored by sleep has proven difficult to explain.
 Sleep efficiency in older adults. Sleep deprivation increases amyloid-β (Aβ) concentrations in the interstitial fluid of experimental animal models and in cerebrospinal fluid in humans, while increased sleep decreases Aβ. Sleep abnormalities may therefore represent a risk factor for neurodegeneration.
Sleep efficiency in older adults. Sleep deprivation increases amyloid-β (Aβ) concentrations in the interstitial fluid of experimental animal models and in cerebrospinal fluid in humans, while increased sleep decreases Aβ. Sleep abnormalities may therefore represent a risk factor for neurodegeneration.
It has recently been shown that sleep is likely a time for clearing waste in the brain or repairing damaged cells. Circadian sleep-wake rhythm disorders are strong predictors of institutionalization.
During a period of wakefulness, coping with the environment requires increasing the number and strength of connections at the synapses between neurons in the brain. This increased activity increases cellular requirements for energy and materials, leading to cellular stress, a major factor in neurodegenerative diseases, and forcing changes in supporting cells such as glial cells, while hindering learning. During sleep, this synaptic activity is decreased which helps restore cellular health and increase plasticity through negative selection of synapses. This may also explain the benefits of sleep for memory acquisition, consolidation, and integration.
In other words, for the theory of synaptic homeostasis, sleep is “the price we pay for our learning and memory abilities”. Increased synaptic activity reduces the selectivity of neuronal responses and limits the ability to learn. By renormalizing synaptic activity, sleep reduces the plasticity burden of neurons and other cells while restoring neuronal selectivity and the ability to learn, and the consolidation and integration of memories.
A new study has just confirmed this, at least in translucent zebrafish larvae. However, these results obtained with zebrafish larvae should only be extrapolated with great caution to humans, but it is nevertheless an interesting discovery for fundamental neuroscience. The study authors used in vivo synaptic labeling tools in larval zebrafish to image the same neurons and their synapses repeatedly over long periods, allowing them to map the synapse changes of a single neuron in states of sleep and wakefulness. In effect, this meant genetically modifying these neurons to allow fluorescence upon firing.
By tracking the synapses of single tectal neurons across sleep-wake states and circadian time, scientists resolve several outstanding questions about the magnitude, universality, and mechanisms of sleep-related plasticity.
They show that synaptic dynamics are present in many cells on average, but when examined neuron by neuron, more diverse patterns of synaptic changes are revealed. These observations may explain some discrepancies between previous studies on the synaptic homeostasis hypothesis, as such single-neuron synaptic dynamics were not captured by one-time snapshots of synapse number or function at the population level.
The authors also found that sleep-related synapse loss depends on molecular signals related to elevated sleep pressure and, notably, also reflects slow-wave activity by occurring primarily at the beginning of the sleep period. This finding raises the question of whether sleep periods associated with low sleep pressure, such as in the second half of the night, play an additional role in non-synaptic remodeling.
Despite all this work was carried out on zebrafish larvae equipped with genetically modified neurons. Thus, any extrapolation to mammals, without even thinking about humans, is highly speculative. Still, it's another clue that sleep is an integral part of good neuronal health, probably along with vascular health and physical activity.

 These articles provide the reader with several points for further reflection.
- One of them is that the clinical trial cannot be the only method of validating the marketing of a drug. Indeed, for diseases that develop over decades, often asymptomatically, how can the effectiveness of a drug be tested? We can always dream of a pill that will cure in a few months a patient, as this is true for diseases where there is an identified pathogen, but it is very unlikely with chronic diseases. Even for communicable diseases, this type of medication does not always exist; a patient can be considered permanently cured, even though they suffer very serious after-effects.
These articles provide the reader with several points for further reflection.
- One of them is that the clinical trial cannot be the only method of validating the marketing of a drug. Indeed, for diseases that develop over decades, often asymptomatically, how can the effectiveness of a drug be tested? We can always dream of a pill that will cure in a few months a patient, as this is true for diseases where there is an identified pathogen, but it is very unlikely with chronic diseases. Even for communicable diseases, this type of medication does not always exist; a patient can be considered permanently cured, even though they suffer very serious after-effects. The exact reasons why atrial fibrillation (a common heart disease) increases dementia risk aren't fully understood, but there are likely several factors involved. Some of these factors directly cause damage, while others increase the chances of getting dementia over time. These factors include tiny blood blockages and bleeding in the brain's small blood vessels. Small strokes you might not even notice, reduce blood flow to the brain, increase long-term inflammation, and lead to shrinkage of brain tissue.
The exact reasons why atrial fibrillation (a common heart disease) increases dementia risk aren't fully understood, but there are likely several factors involved. Some of these factors directly cause damage, while others increase the chances of getting dementia over time. These factors include tiny blood blockages and bleeding in the brain's small blood vessels. Small strokes you might not even notice, reduce blood flow to the brain, increase long-term inflammation, and lead to shrinkage of brain tissue.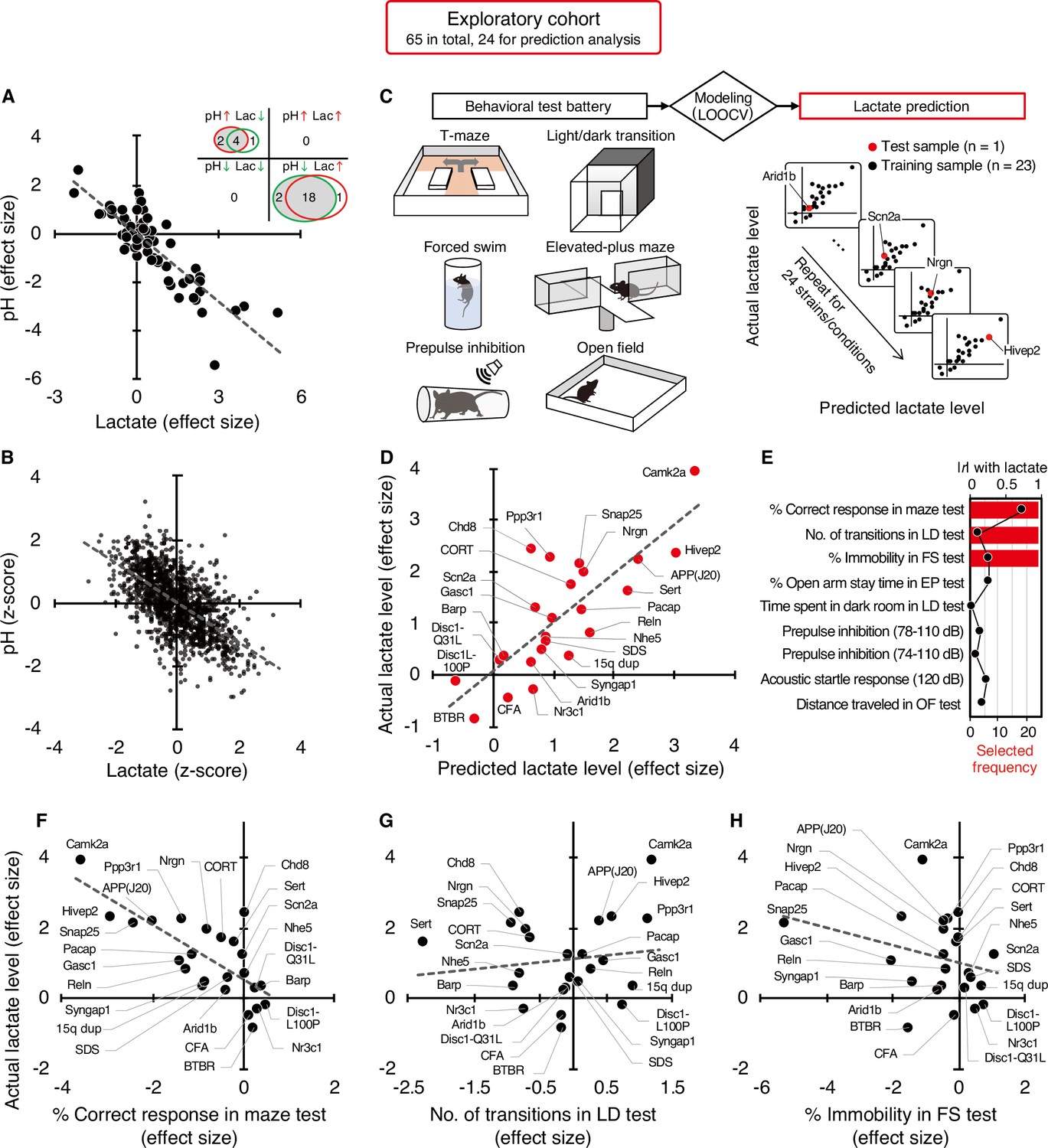 What could be the mechanism between increased lactate and decreased pH?
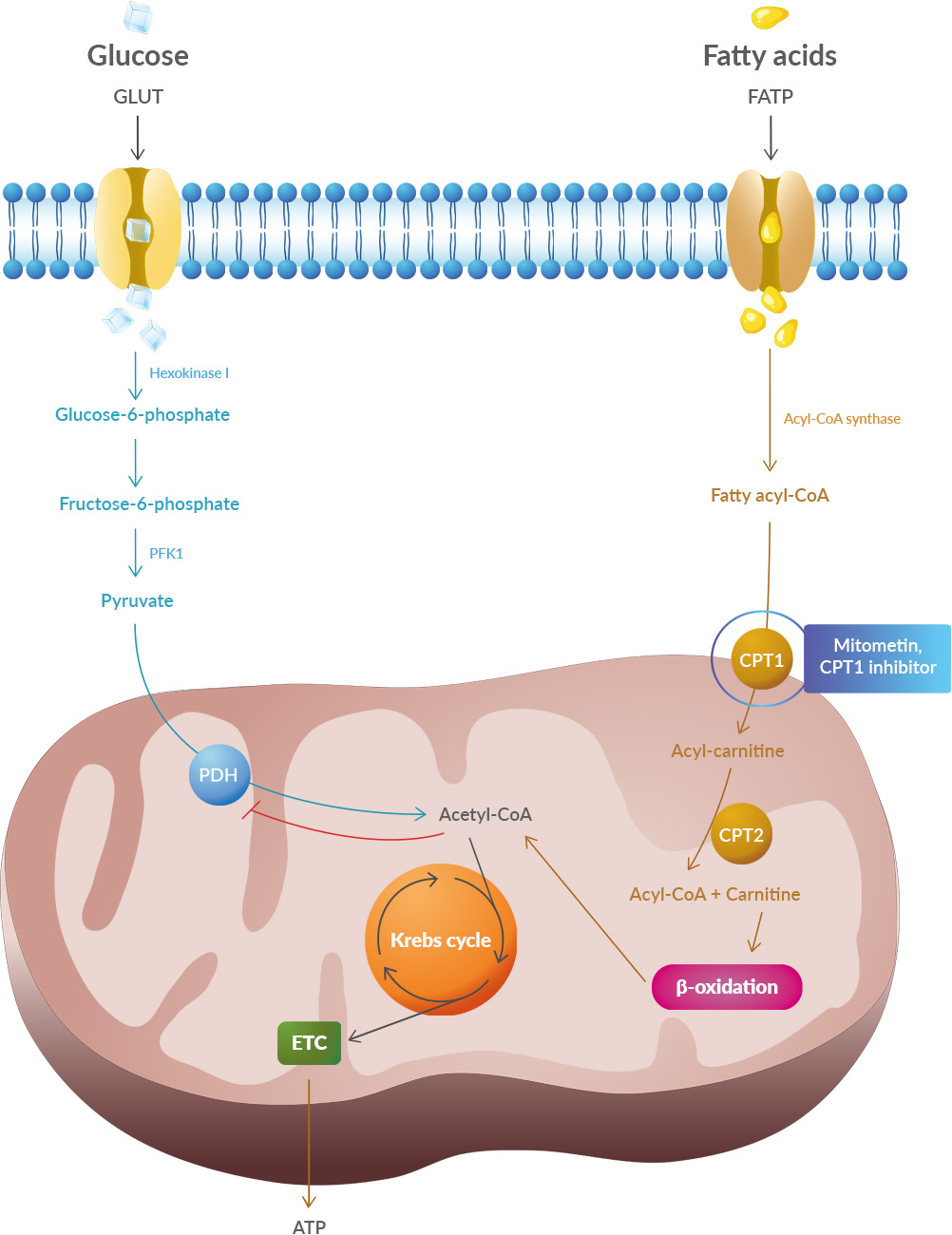
Lactate is a byproduct of metabolism and it is an acid, hence the acidification of pH. Neuronal activity relies heavily on glucose for energy. Under normal conditions, oxygen is readily available, and glucose is broken down through aerobic respiration, producing ATP (energy) with minimal lactate as a byproduct. However, during periods of high neuronal activity or limited oxygen supply, cells shift to anaerobic metabolism, relying more on glycolysis. This process produces more lactate as a byproduct.
What could be the mechanism between increased lactate and decreased pH?
Lactate is a byproduct of metabolism and it is an acid, hence the acidification of pH. Neuronal activity relies heavily on glucose for energy. Under normal conditions, oxygen is readily available, and glucose is broken down through aerobic respiration, producing ATP (energy) with minimal lactate as a byproduct. However, during periods of high neuronal activity or limited oxygen supply, cells shift to anaerobic metabolism, relying more on glycolysis. This process produces more lactate as a byproduct. Improving cognition using a simple probiotic would be an extraordinary result due to its simplicity of implementation.
Improving cognition using a simple probiotic would be an extraordinary result due to its simplicity of implementation.
 Studies have shown that oxidative stress and endoplasmic reticulum stress are correlated and can lead to protein misfolding (Abramov et al., 2020). Accumulation of misfolded proteins causes cellular damage and mitochondrial dysfunction and is associated with a range of neurodegenerative diseases, including ALS (misfolded SOD1, TDP-43, C9orf72) (McAlary et al., 2020), Parkinson's disease (misfolded α-synuclein) and Alzheimer disease (misfolded Aβ and Tau) (Abramov et al., 2020).
Studies have shown that oxidative stress and endoplasmic reticulum stress are correlated and can lead to protein misfolding (Abramov et al., 2020). Accumulation of misfolded proteins causes cellular damage and mitochondrial dysfunction and is associated with a range of neurodegenerative diseases, including ALS (misfolded SOD1, TDP-43, C9orf72) (McAlary et al., 2020), Parkinson's disease (misfolded α-synuclein) and Alzheimer disease (misfolded Aβ and Tau) (Abramov et al., 2020).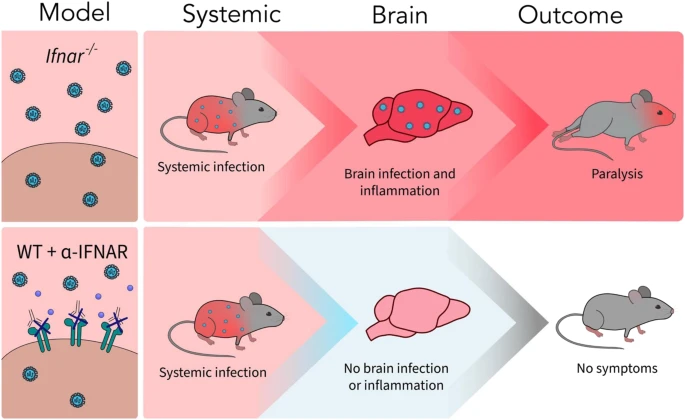 A new article aims to show that in the case of Zika viruses,
A new article aims to show that in the case of Zika viruses, 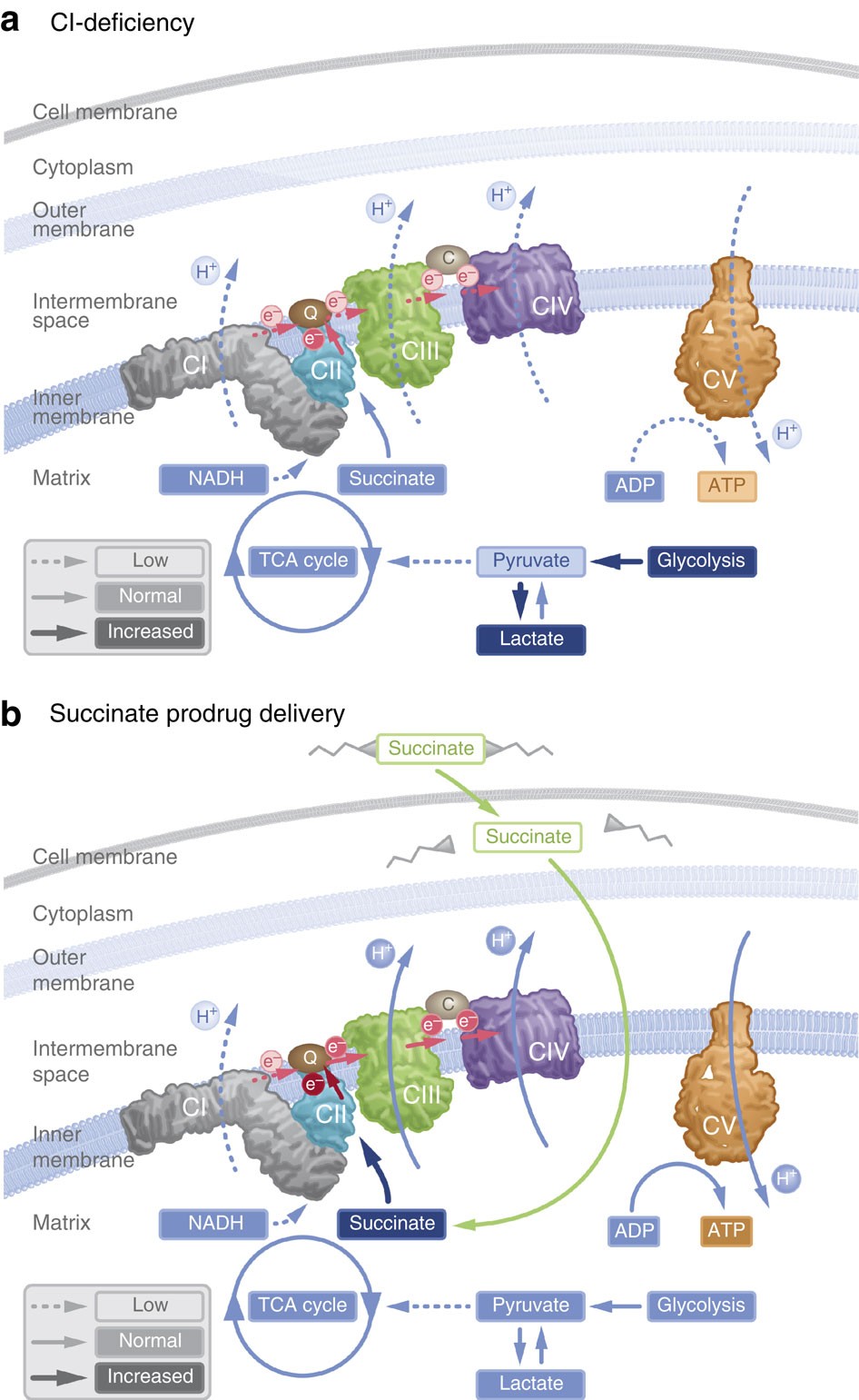 In particular, supplementation with dimethyl succinate, a substrate bypassing the inhibited step in the TCA cycle, suggests a potential therapeutic strategy to mitigate mitochondrial dysfunction in Alzheimer's disease. Dimethyl succinate (DMS), a membrane-permeant form of succinate, could serve as a pro-drug to provide substrate to the next enzymatic step in the TCA cycle, succinate dehydrogenase (SDH).
In particular, supplementation with dimethyl succinate, a substrate bypassing the inhibited step in the TCA cycle, suggests a potential therapeutic strategy to mitigate mitochondrial dysfunction in Alzheimer's disease. Dimethyl succinate (DMS), a membrane-permeant form of succinate, could serve as a pro-drug to provide substrate to the next enzymatic step in the TCA cycle, succinate dehydrogenase (SDH).