The level of interest and knowledge among scientists about human physiology and anatomy is appalling.
We know that higher primates (including humans) have a special corticospinal system for dealing with tasks that need high skills. Most animal models of ALS do not have this kind of corticospinal system. Another feature of this corticospinal system in higher primates is that the connection from upper motor neurons to lower motor neurons is done directly in some cases (for example the hands), while in most animals the interconnection is done with interneurons, which take in charge automatic and repetitive movements such as walking.
Yet publications are still written that discuss at length of interneurons' role in ALS. One such publication (a review) is interesting as it starts well, by stating the obvious, that as there were hundreds of unsuccessful clinical trials on ALS drugs, we must have missed something important.
 Alas, the authors resort to an old hypothesis, one of the first about ALS etiology, which is the excitotoxicity hypothesis.
Alas, the authors resort to an old hypothesis, one of the first about ALS etiology, which is the excitotoxicity hypothesis.
This old hypothesis postulates that increased activation of upper motor neurons spreads pathology to lower motor neurons in the spinal cord in the form of excessive glutamate release, which triggers excitotoxic processes. As the authors recall many clinical trials have focused on therapies that target excitotoxicity via dampening neuronal activation, but not one was effective.
On the contrary, the authors never mentioned that the only clinical trials that were successful were about mutations in some rare cases (SOD1). A few other clinical trials did better than the average but they were far from providing a cure, they addressed cellular stress. It seems obvious now that for the majority of ALS patients, the cellular stress response is defective.
The authors correctly state that the current evidence requires revision in the context of appreciating the complexity of the nervous system and the limitations of the neurobiological assays the scientists use to study it.
The authors ask for more research:
Network activity: Assess the activity level of the affected networks, not just excitability.
Individual neurons: Investigate how ALS pathology affects the function of individual neurons, including lower motor neurons and interneurons.
Interneurons: Understand their role and how their activity changes in ALS.
Point 1. looks like we are still in the 1940' with the Nernst and Goldman equations.
Point 2. is about the function of individual neurons. That's weird, people are not made of individual neurons, neuron types are numerous and are not even the sole cell population, and there are many more non-neuronal cells than neurons in the CNS. All these cells type collaborate and compete in what we call "tissue".
Point 3. is weird, ALS strikes a special kind of muscle (skeletal muscles) and nerves (corticospinal). In most cases, the lower motor neurons that connect to these muscles are not themself connected to an interneuron.
What to conclude from this review? I assume the authors are in good faith, but by perpetrating obsolete ideas they slow any progress toward a cure for ALS

 Cortico-motoneuronal projection is a late evolutionary development that is present only in dexterous primates, such as capuchins, macaques, great apes, and humans, but absent in adult rodents, carnivores, and many others. primates, such as marmosets.
Cortico-motoneuronal projection is a late evolutionary development that is present only in dexterous primates, such as capuchins, macaques, great apes, and humans, but absent in adult rodents, carnivores, and many others. primates, such as marmosets. What is interesting is that 14-3-3θ seems to interact preferentially with pathogenic TDP-43 versions but not with the usual version of TDP-43. This suggests that reducing the production (or increasing the degradation) of 14-3-3θ would reduce the production of pathogenic TDP-43. Scientists have therefore sought to reduce the amount of this 14-3-3θ protein in cells through genetic therapy.
What is interesting is that 14-3-3θ seems to interact preferentially with pathogenic TDP-43 versions but not with the usual version of TDP-43. This suggests that reducing the production (or increasing the degradation) of 14-3-3θ would reduce the production of pathogenic TDP-43. Scientists have therefore sought to reduce the amount of this 14-3-3θ protein in cells through genetic therapy.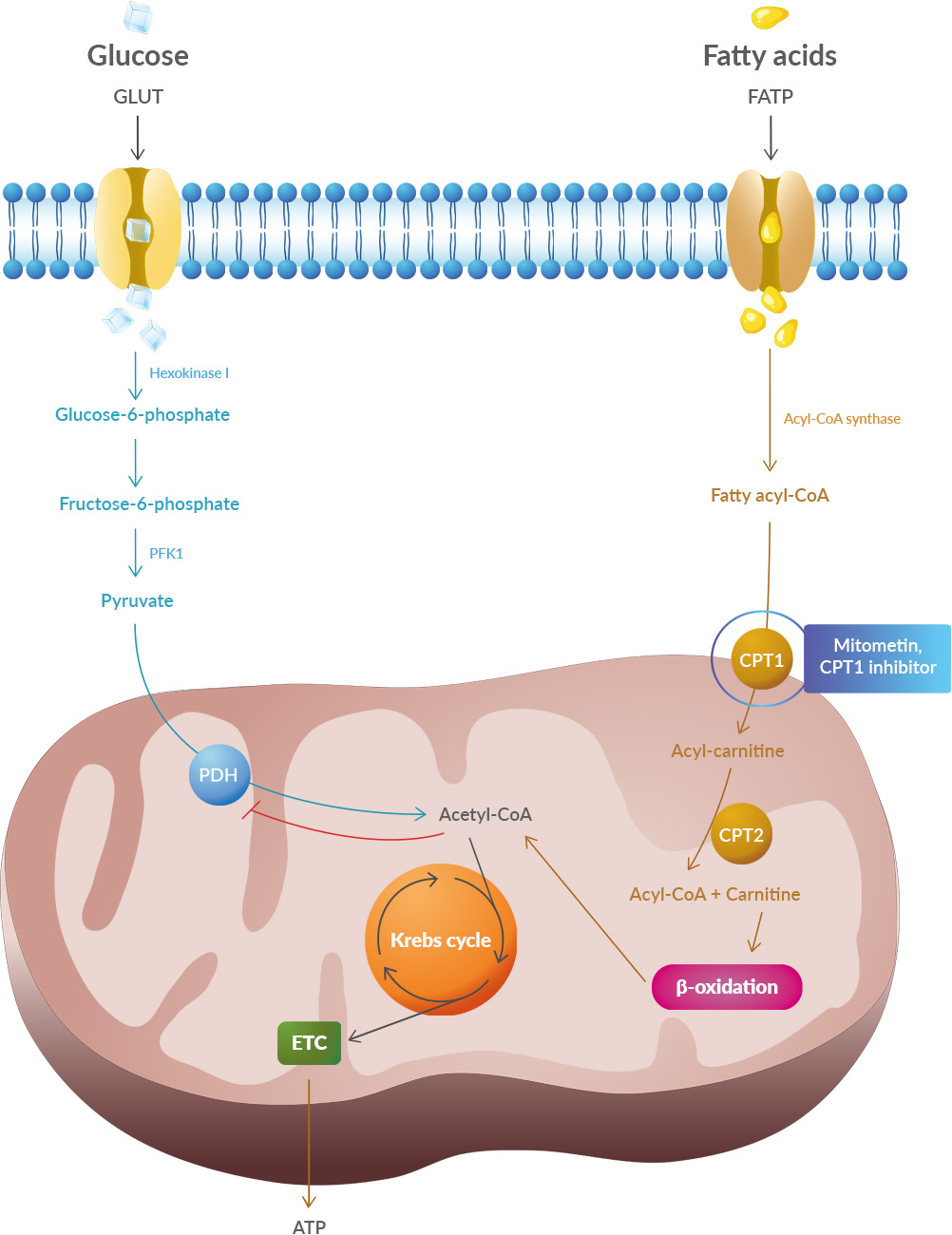 Studies have shown that oxidative stress and endoplasmic reticulum stress are correlated and can lead to protein misfolding (Abramov et al., 2020). Accumulation of misfolded proteins causes cellular damage and mitochondrial dysfunction and is associated with a range of neurodegenerative diseases, including ALS (misfolded SOD1, TDP-43, C9orf72) (McAlary et al., 2020), Parkinson's disease (misfolded α-synuclein) and Alzheimer disease (misfolded Aβ and Tau) (Abramov et al., 2020).
Studies have shown that oxidative stress and endoplasmic reticulum stress are correlated and can lead to protein misfolding (Abramov et al., 2020). Accumulation of misfolded proteins causes cellular damage and mitochondrial dysfunction and is associated with a range of neurodegenerative diseases, including ALS (misfolded SOD1, TDP-43, C9orf72) (McAlary et al., 2020), Parkinson's disease (misfolded α-synuclein) and Alzheimer disease (misfolded Aβ and Tau) (Abramov et al., 2020).
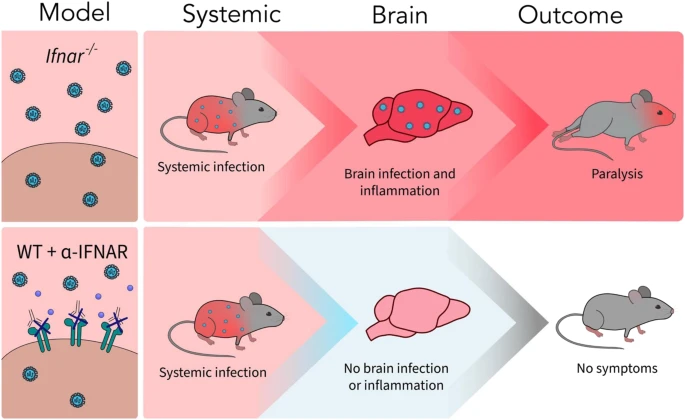 A new article aims to show that in the case of Zika viruses,
A new article aims to show that in the case of Zika viruses,  Yichang Jia, Ph.D., Co-founder of SineuGene
Yichang Jia, Ph.D., Co-founder of SineuGene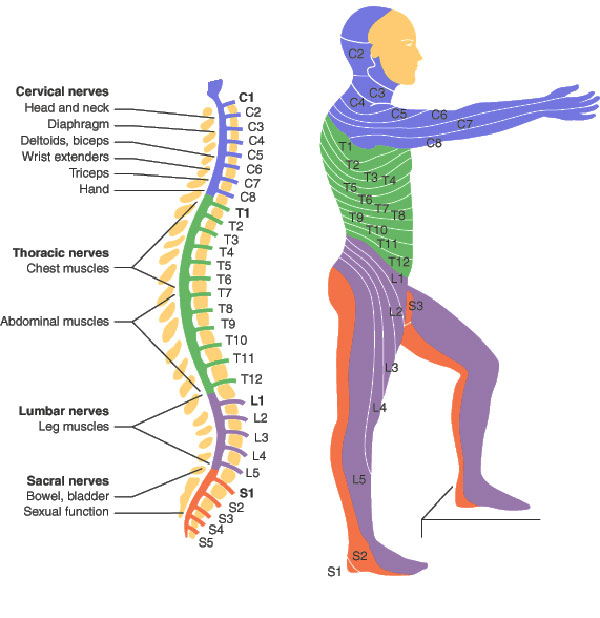 Obviously, a spinal cord injury will sever the link between the brain motor area, some upper motor neurons, and corresponding lower motor neurons and muscles. Yet it does not stop there, which is particularly interesting when we have ALS in mind. In spinal-onset ALS the disease starts in a very localized muscular for example a muscle in the thumb, and it spreads, often until respiratory muscles fail.
Obviously, a spinal cord injury will sever the link between the brain motor area, some upper motor neurons, and corresponding lower motor neurons and muscles. Yet it does not stop there, which is particularly interesting when we have ALS in mind. In spinal-onset ALS the disease starts in a very localized muscular for example a muscle in the thumb, and it spreads, often until respiratory muscles fail.