As a layperson I have been studying ALS by reading scientific publications for several years, it started after the second time someone went ill in my family. This blog is the result of that effort. Scientists claim to find cures for most chronic diseases every week by targeting one or the other obscure molecule. We know that most of these articles are of very poor quality. What feels important to me are articles that show a good knowledge of human anatomy and physiology. I don't care about molecules in mice.
Nearly one century ago, medical doctors made a parallel between spinal cord injury and spinal-onset ALS. In both cases, there is important muscle wasting.
And this is what kills people, so it's important to understand how this develops and what are the consequences.
 Obviously, a spinal cord injury will sever the link between the brain motor area, some upper motor neurons, and corresponding lower motor neurons and muscles. Yet it does not stop there, which is particularly interesting when we have ALS in mind. In spinal-onset ALS the disease starts in a very localized muscular for example a muscle in the thumb, and it spreads, often until respiratory muscles fail.
Obviously, a spinal cord injury will sever the link between the brain motor area, some upper motor neurons, and corresponding lower motor neurons and muscles. Yet it does not stop there, which is particularly interesting when we have ALS in mind. In spinal-onset ALS the disease starts in a very localized muscular for example a muscle in the thumb, and it spreads, often until respiratory muscles fail.
Similarly, a spinal cord injury has consequences that are far from being limited to some motor neurons and diseases. For example, pulmonary infection is a leading cause of morbidity after spinal cord injury. Bizarrely this happens because spinal cord injury causes atrophy and dysfunction in the lymphatic system, an organ system in vertebrates that is part of the immune system.
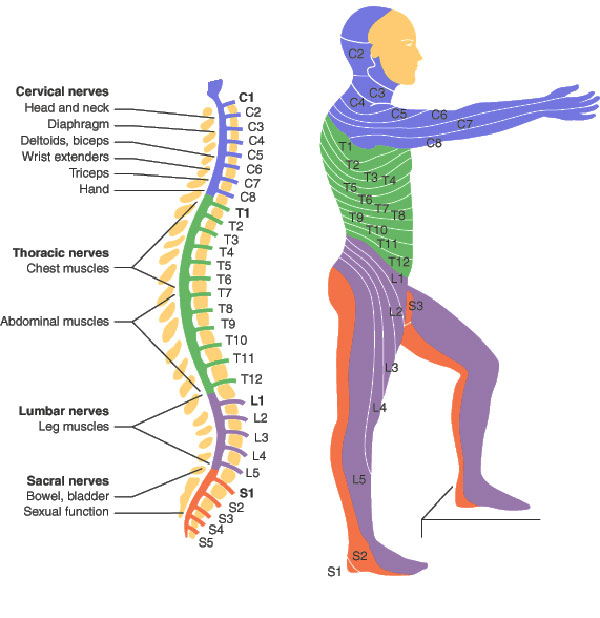
Now scientists from Ohio, describe systemic wasting that affects innervated non-paralyzed skeletal muscles. The muscles that are affected in ALS are also skeletal muscles. This wasting appeared within 1 week after experimental spinal cord injury in mice and in three weeks half of the muscle mass disappeared. This waste affects the whole body. Skeletal muscle fibers are broadly classified as "slow-twitch" (type 1) and "fast-twitch" (type 2). This muscle wasting affects fast type 2 muscles preferentially, and became exacerbated after a third thoracic vertebra (T3) paraplegia compared with low (T9) thoracic paraplegia. The T3 vertebra is situated at the level of the shoulder, while the T9 is at the height of the sternum.
Markus E. Harrigan, Jan M. Schwab et al. remark that the wasting of nonparalyzed muscle and its rapid onset and severity cannot be explained by disuse, so it implies unknown systemic drivers. Mechanisms underlying systemic muscle wasting (including fully innervated non-paralyzed muscles) early after paraplegic SCI would imply the presence of biological signaling which can quickly reach muscles of the entire body. Knowing the cause of this widespread muscle wasting after a T3 paraplegia in spinal cord injury might illuminate the similar phenomena in ALS.
The authors found that muscle transcriptome and biochemical analysis revealed a glucocorticoid-mediated catabolic signature early after T3 spinal cord injury. They generated an inducible skeletal muscle-specific glucocorticoid receptor (GR) knockout mouse model in order to test that hypothesis.
Spinal cord injury-induced systemic muscle wasting was mitigated by (i) endogenous glucocorticoid ablation (adrenalectomy) and (ii) pharmacological glucocorticoid receptor (GR) blockade and was (iii) completely prevented after T3 relative to T9 spinal cord injury by genetic muscle-specific GR deletion.
These results suggest that hypercortisolism contributes to a rapid systemic and functionally relevant muscle wasting syndrome early after paraplegic spinal cord injury in mice. Indeed in humans, hypercortisolism induces central muscle weakness, adipose tissue redistribution, skin fragility and unusual infections. Hypercortisolism has also been implicated in ALS, maybe it would be interesting to test glucocorticoid inhibitors in a clinical trial. There are studies (here or here) that show that glucocorticoid inhibitors ameliorated the health in an ALS mice model.
