History of brain organoids
Cerebral organoids have provided a means of generating complex, three-dimensional and in vitro models of human neurons that summarize, in part, neuronal diversity and aspects of the physical architecture of the developing brain, such as stratification.
The researchers led by Lancaster generated the first cortical organoids in 2013. They seeded stem cells in a three-dimensional matrix with a nutrient bath. Within a month, the cells have differentiated and formed small structures of a few millimeters, looking like miniature brains. These cell layers mimicked structures such as the hippocampus and cerebral cortex. Without blood supply, however, the neurons at the center of these organoids decayed and eventually died.
The brain organoids as models
The organoids of the human brain have become a promising model for the study of neural development and neurological disorders, including Alzheimer's disease. This model has enormous potential for testing therapeutic agents and determining their permeability across the blood-brain barrier.
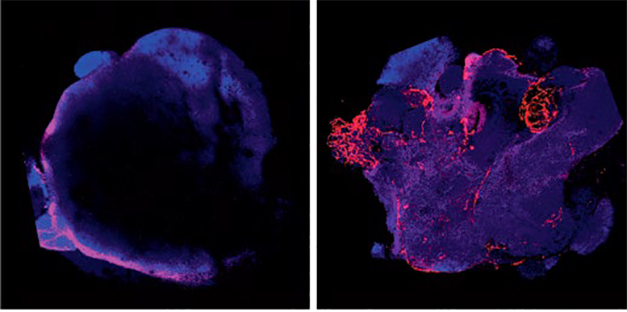
However, it remains difficult to generate an authentic model that summarizes the complex structure and function of the human brain. Brain organoids can not fully capture the cellular diversity of the brain. The absence of microglia and blood vessels is particularly troublesome, if one wants to apply these organoids to the study of Alzheimer's disease. The absence of a vascular system causes the organoids to become limited in size and contain a largely necrotic nucleus due to the inability of the nutrient fluid to enter the center of the structure.
What is the contribution of Cakir and his colleagues?
Cakir and his colleagues established an organo-cerebral model with a vascular-like system that works in implanted mice. This system is unique in many respects compared to previously published brain organoids.
They generated vascularized human cortical organoids by expressing an endothelial transcription factor. They discovered that such human cortical organoids developed a complex vascular network. The vascularized human cortical organoids were in good health compared to nonvascularized equivalent organoids.
When the authors compared cellular transcriptomes, they found that vascularized human cortical organoids expressed more mature neuronal markers, as well as markers of other cell types, particularly those involved in the formation of neurovascular units. including tight junction markers, astrocyte and pericytic proteins, and transporters.
Application to Alzheimer's disease
In addition, the treatment of vascularized human cortical organoids with oligomeric Aβ42 resulted in tight junction malformation and disruption of the blood-brain barrier, indicating that the blood-brain barrier structure responds to exogenous factors. The vascularized human cortical organoids were grafted into mice and formed functional vascular connections with the host mouse.
With respect to Alzheimer's disease, the authors have shown that oligomeric synthetic Aβ preparations selectively perturb the permeability of the blood-brain barrier in their vascularized human cortical organoids. An interesting question is: Is it possible that high levels of oligomeric Aß could compromise cerebrovascular integrity and allow therapeutic biological products and small molecules to pass freely across the blood-brain barrier of patients with Alzheimer's disease?
How to apply brain organoids technology to the study of neurodegenerative diseases?
First, given the known variability among organoids, future studies should address the fundamental issue of reproducibility and functional homogeneity. In addition, the current method for modeling fetal brain-like organoids may be somewhat limited for summarizing a mature brain environment. The vasculature of the adult brain is much more complex, including in the perivascular spaces, which contribute to the elimination of toxic solutes such as Aβ.
The incorporation of iPSC microglia into organoids (Abud et al., 2017), paves the way for the creation of complex, multicellular and human in vitro models to study the mechanisms of non-cellular autonomic diseases in Alzheimer.
It will be very interesting now to investigate whether the blood vessels are able to constrict and dilate, if the pericytes can contract and relax, if the vascularized human cortical organoids would be useful for studying neurovascular coupling, if there is venous and arterial flow and many others questions. The next years of research using vascularized brain organoids will provide more answers and will undoubtedly enable many breakthroughs in the cerebrovascular field.
http://www.ncbi.nlm.nih.gov/pubmed/31591580

