Japanese scientists, including the famous ALS specialist Makoto Urushitani, as well as the first author Ryutaro Nakamura, wanted to study whether hypermetabolism, but also lipid metabolism, could predict the prognosis of patients with Early amyotrophic lateral sclerosis (ALS), with different nutritional profiles when they are hospitalized.

Indeed, many elements show the importance of non-pharmacological treatment which can improve quality of life, decrease progression or increase survival time in ALS.
The early introduction of non-invasive positive pressure ventilation, especially with cough assistants, would prolong the life of ALS.
In addition, a high calorie diet effectively slows the progression of ALS, especially in patients with rapid progression.
Surprisingly, in rapidly progressing ALS, a fat-dominant high calorie diet inhibits the elevation of serum neurofilament-L (NFL), a convincing biomarker of neuronal damage.
A body mass index (BMI) of less than 18.5 on the first visit to neurologists is recognized as a factor of poor prognosis.
Despite these clinical evidence, and although many studies have shown that age and BMI are the best biomarkers for predicting the course of ALS, these studies encounter a sort of consensus narrative barrier that says ALS is a disease of the upper motor neurons and the loss of muscle mass is exclusively due to the lack of activation by the lower motor neurons.
Similarly while scientists say that TDP-43-like proteopathy is present in all cells of the body of patients, particularly in skeletal muscles (those involved in ALS) in 97% of cases, it seems it is unlikely that ALS would target only certain cells and only in the brain and spinal cord.
Finally, more than half of ALS patients have hypermetabolism, that is, to perform a certain task, their body needs more energy than the body of a healthy person.
Patients with ALS have impaired glucose tolerance from an early stage, and free fatty acids are higher in these patients than in those with normal glucose tolerance. The energy production pathway has been reported to switch from glycolytic metabolism to lipid metabolism during disease.
This indicates that lipids could be the primary fuel in malnourished patients as well as in ALS mice, although no studies have examined changes in metabolism in response to nutritional status in humans.
Elevated levels of total and low density lipoprotein (LDL) cholesterol and a higher LDL / high density lipoprotein (HDL) cholesterol ratio have been associated with longer survival, which could indicate a metabolism primarily using lipids rather than glucose.
Therefore, Ryutaro Nakamura and colleagues retrospectively reviewed the available information on forty-eight patients (25 men; 23 women) over 49 years of age with ALS admitted to Shiga University of Medical Sciences Hospital. from March 2018 to February 2021.
The aim of the scientists was to test the hypothesis that the impact of hypermetabolism on survival might differ depending on nutritional status.
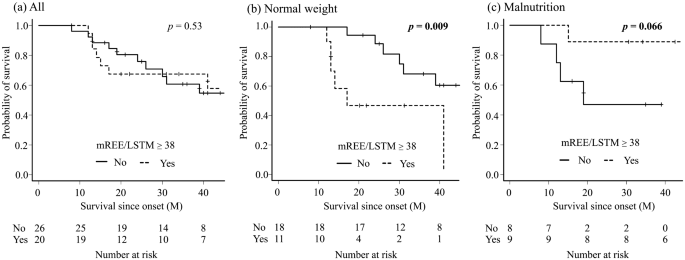
Fig. 1: Comparison of the survival rate between the hypermetabolic group and the normal metabolic group in all patients (a), the normal weight group (b), the malnutrition group (c). Kaplan-Meier analyzes and the log-rank test showed that there was no difference in all patients; however, the hypermetabolic group had a significantly shorter survival time in the normal weight group and a longer survival time in the malnutrition group, although the difference was not significant.
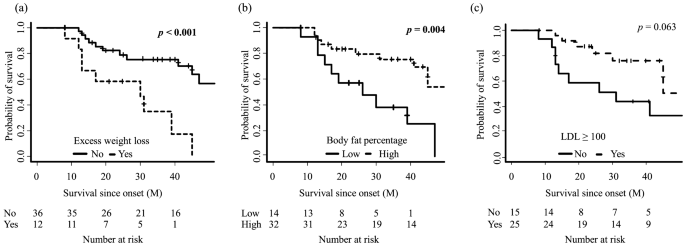
Fig. 2: Comparison of survival rate between patients with amyotrophic lateral sclerosis stratified by excessive weight loss (a), body fat percentage (b) and low density lipoprotein (LDL) cholesterol (c). analyzes showed that patients with excessive weight loss and a low percentage of body fat had a significantly shorter survival time.
In this study, Japanese scientists explored the effect of hypermetabolism on survival versus nutritional status of patients with ALS, and found that hypermetabolic patients with normal weight had a shorter life, while survival was longer in hypermetabolic patients with malnutrition. They find that survival is correlated with LDL levels.
The low level of skeletal muscle and soft tissue mass, which is a factor of poor prognosis, could be the reason why the prognosis of the normal weight hypermetabolic group is worse than that of the other groups.
Surprisingly, hypermetabolism was a better prognostic factor in the malnutrition group (Fig. 1). Lipid biomarkers were characteristic in this group, which may contribute to longer survival.
The hypermetabolic malnutrition group had the highest median LDL value among all groups, and a higher body fat percentage, which were good prognostic factors in previous studies.
Indeed, patients with a high body fat percentage had a longer survival in their study (Fig. 2), and patients with high LDL showed a similar trend.
It should be noted that the respiratory quotient was less than 0.85 in eight of the nine patients in this group and that the fasting blood sugar was significantly higher in this group, which could indicate a change in lipid metabolism compared to the glucose hypothesis.
Respiratory quotient was associated with ALSFRS-R and time from onset, and it is interesting to hypothesize that a "fuel switch" may underlie metabolic profiles in progression. of ALS.
In addition, Steyn et al. reported that high fatty acid oxidation increases whole body energy expenditure and slows disease progression, which may support the findings described here and indicate the contribution of hyperlipid metabolism to longer survival. these results caution against measuring hypermetabolism as the only prognostic indicator.
Based on the possible involvement of skeletal muscle hypermetabolism in the prognosis of ALS, Japanese scientists propose the following equation "BMM = (BMI - 19.8) × (mREE / LSTM - 38)", which successfully predicted the prognostic factor regardless of nutritional status. BMM = BMI-muscle metabolism mREE = measured rest energy expenditure LSTM = lean soft tissue mass
In conclusion, these studies show that a weight loss of more than 10% was a factor of poor prognosis. The rate of weight loss was faster in the high BMM group; thus, the BMM index could be a valuable indicator for considering aggressive nutritional intervention, including PEG (percutaneous endoscopic gastrostomy), at an early stage of clinical practice.
Calorie supplementation high in fat or carbohydrate is still a matter of debate. Some reports suggest that high-fat calorie supplementation is a better nutritional treatment in patients with ALS, while others recommend high-carbohydrate calorie supplementation.
For patients with chronic obstructive pulmonary disease who have reduced CO2 emissions, a high fat diet is recommended because lipid metabolism produces less carbon dioxide. Based on their finding that the tendency to alter lipids might contribute to a better prognosis, a high fat intake might be an attractive option in a high calorie diet for ALS. Of course, the choice of nutrition should be made with caution, depending on the metabolic profiles of the patients.
The definition the authors adopted for hypermetabolism is a high mREE / LSTM, rather than the popular world index, mREE / pREE, as the PRE estimated by the Harris-Benedict equation would not be appropriate for the assessment. metabolic rate of the Japanese.
